5 Steps To Prevent Medical Billing Fraud Embezzlement
5 Steps To Prevent Medical Billing Fraud Embezzlement How to prevent healthcare fraud. although no practice is 100% safe, there are a few simple protocols that can be made to ensure heightened awareness and prevent financial loss. segregate duties within the finance function – make sure that the individual responsible for collecting payments is separate from the individual that deposits them. Cms categorizes fraud and program integrity issues into 4 categories: (1) mistakes resulting in administrative errors, such as incorrect billing; (2) inefficiencies causing waste, such as ordering excessive diagnostic tests; (3) bending and abuse of rules, such as upcoding claims; and (4) intentional, deceptive fraud, such as billing for.
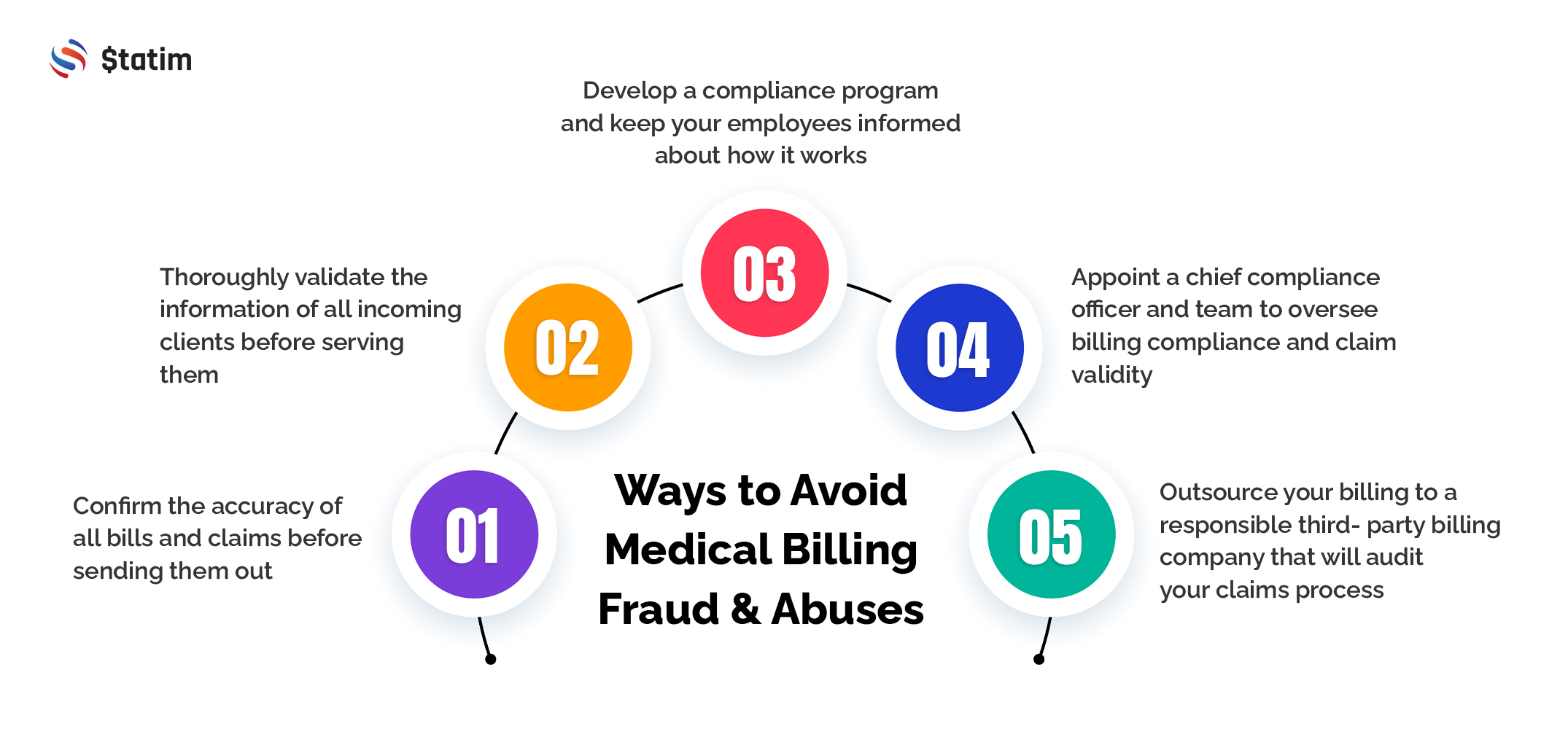
How To Avoid Medical Billing Fraud Abuses And Errors Statim Llc The best way to protect your workplace from fraud and abuse is to have a compliance program. large health care organizations have had these in place for years and physician employees should be aware of their responsibilities in the program. with the passage of the patient protection and affordable care act of 2010, physicians who treat medicare. Common types of health care fraud fraud committed by medical providers. double billing: submitting multiple claims for the same service phantom billing: billing for a service visit or supplies the. How to prevent fraud and abuse in healthcare. step 1: identify potentially fraudulent practices. step 2: understand current healthcare regulations. step 3: maintain good data security. step 4: audit your ordering and billing frequently. step 5: create a compliance plan. Everyone shares the burden of health care fraud. in 2018, $3.6 trillion was spent on health care in the united states, representing billions in health insurance claims. it is an undisputed reality that some of these claims are fraudulent. although they constitute only a small fraction, those fraudulent claims carry a very high price tag, both.

Ways To Prevent Medical Billing Fraud Medconverge How to prevent fraud and abuse in healthcare. step 1: identify potentially fraudulent practices. step 2: understand current healthcare regulations. step 3: maintain good data security. step 4: audit your ordering and billing frequently. step 5: create a compliance plan. Everyone shares the burden of health care fraud. in 2018, $3.6 trillion was spent on health care in the united states, representing billions in health insurance claims. it is an undisputed reality that some of these claims are fraudulent. although they constitute only a small fraction, those fraudulent claims carry a very high price tag, both. The objectives of this commentary are to describe the types and trends of medicare and medicaid fraud that are committed, and provide recommendations to protect patients and health care practices. specifically, this article identifies types of medicare and medicaid fraud at beneficiary (patient) and provider level, and it can be intentional or. The diference between “fraud” and “abuse” depends on specific facts, circumstances, intent, and knowledge. examples of medicare abuse include: billing for unnecessary medical services. charging excessively for services or supplies. misusing codes on a claim, such as upcoding or unbundling codes.
How To Avoid Medical Billing Fraud The objectives of this commentary are to describe the types and trends of medicare and medicaid fraud that are committed, and provide recommendations to protect patients and health care practices. specifically, this article identifies types of medicare and medicaid fraud at beneficiary (patient) and provider level, and it can be intentional or. The diference between “fraud” and “abuse” depends on specific facts, circumstances, intent, and knowledge. examples of medicare abuse include: billing for unnecessary medical services. charging excessively for services or supplies. misusing codes on a claim, such as upcoding or unbundling codes.

Comments are closed.