Pathophysiology Asthma Airway
Understanding Asthma Pathophysiology Diagnosis And Management Asthma is a common chronic disorder of the airways that involves a complex interaction of airflow obstruction, bronchial hyperresponsiveness and an underlying inflammation. this interaction can be highly variable among patients and within patients over time. this section presents a definition of asthma, a description of the processes on which that definition is based—the pathophysiology and. Asthma is becoming a more prevalent disease since the early 1990s. from 1982 to 1992, the rate of asthma jumped from 34.7 to 49.4 per thousand.[1] the prevalence of asthma in the usa is around 8%.[2] there also has been some mixed trends around the world where different countries have either had increasing cases or have been stagnant.[3] in children, asthma is presented predominantly in males.

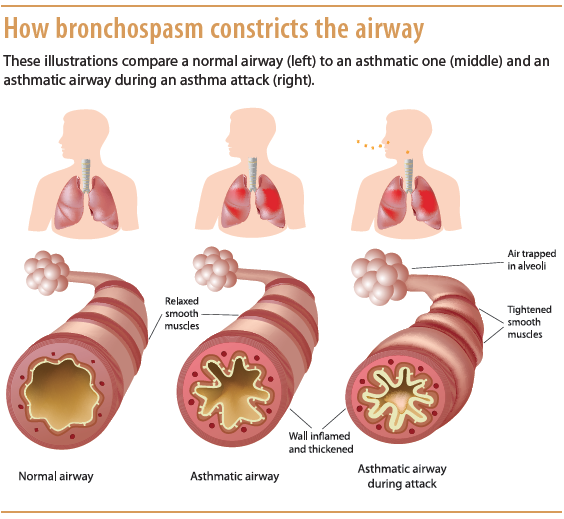
Airway Smooth Muscle Pathophysiology In Asthma Journal Of Allergy And Asthma is a syndrome characterized by diverse underlying mechanisms and involves intricate interactions among inflammatory and resident airway cells. these mechanisms lead to airway inflammation, intermittent airflow obstruction, and bronchial hyperresponsiveness (see image. pathophysiology of asthma). The pathophysiology of asthma is how the disease affects the normal function of the airways. it includes hypersensitivity of the airways, airflow obstruction, and reversibility. however, in some. Pathophysiology. the understanding of the pathophysiology of asthma has advanced in the past decade. it is a condition of bronchial hyperactivity with the inflammatory component central to the pathogenesis of symptoms. asthma is characterized by inflammation of the airways, with an abnormal accumulation of inflammatory cells in the bronchioles. Endobronchial biopsy of proximal airways in severe asthma has shown persistent type 2 inflammation characterized by airway eosinophils, lymphocytes, mast cells and associated thickening of the rbm despite regular use of oral corticosteroids. 80 interestingly, eosinophilia in severe asthma was similar to that in steroid naïve, mild asthma with.

7 Schematic Representation Of Asthma Pathophysiology Several Pathophysiology. the understanding of the pathophysiology of asthma has advanced in the past decade. it is a condition of bronchial hyperactivity with the inflammatory component central to the pathogenesis of symptoms. asthma is characterized by inflammation of the airways, with an abnormal accumulation of inflammatory cells in the bronchioles. Endobronchial biopsy of proximal airways in severe asthma has shown persistent type 2 inflammation characterized by airway eosinophils, lymphocytes, mast cells and associated thickening of the rbm despite regular use of oral corticosteroids. 80 interestingly, eosinophilia in severe asthma was similar to that in steroid naïve, mild asthma with. Obstruction of the lumen of the bronchiole by mucoid exudate, goblet cell metaplasia, epithelial basement membrane thickening and severe inflammation of bronchiole. during an asthma episode, inflamed airways react to environmental triggers such as smoke, dust, or pollen. the airways narrow and produce excess mucus, making it difficult to breathe. Chronic lower airway inflammation is known to be more common in individuals that also have inflammatory disorders of the upper airway. the scientific understanding of asthma continues to improve and it is important for providers who treat upper or lower airway inflammation to be familiar with asthma's definition and pathophysiology.
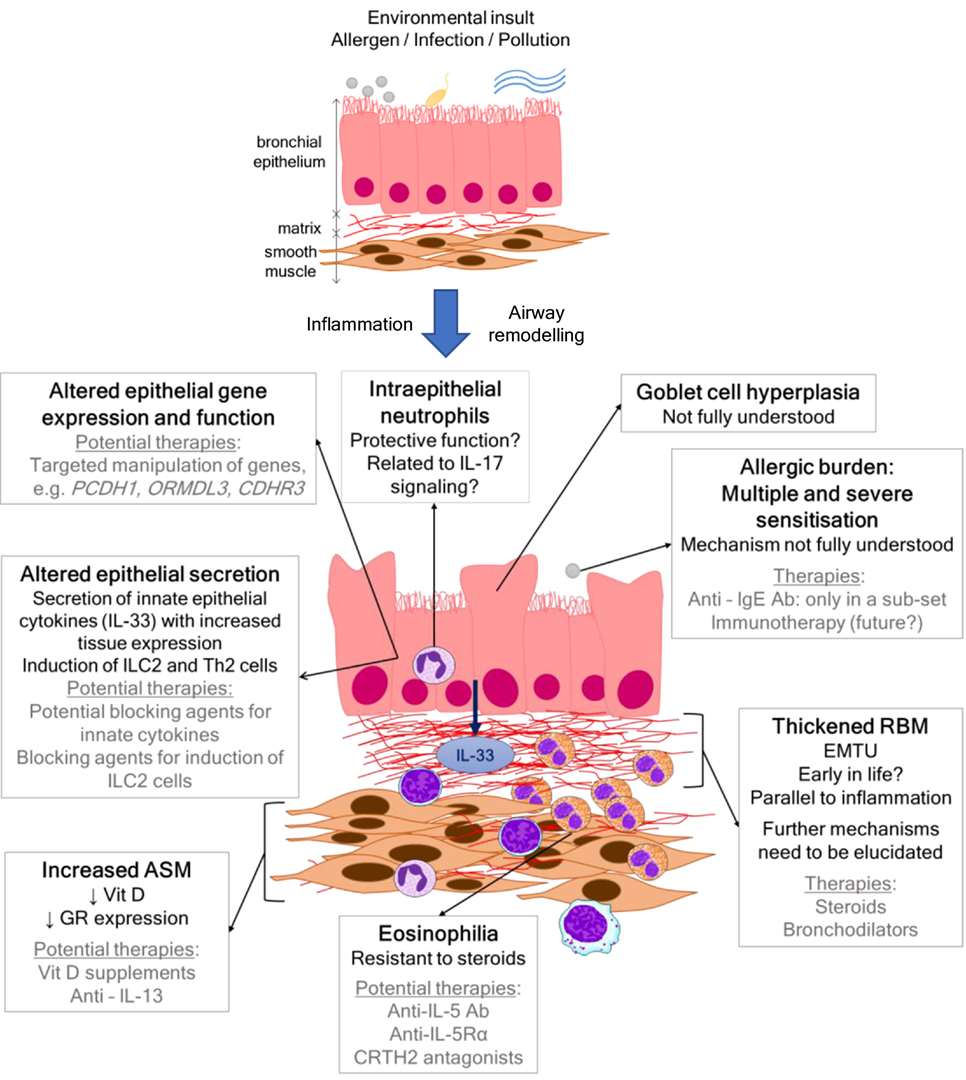
Pathophysiology Asthma Airway Obstruction of the lumen of the bronchiole by mucoid exudate, goblet cell metaplasia, epithelial basement membrane thickening and severe inflammation of bronchiole. during an asthma episode, inflamed airways react to environmental triggers such as smoke, dust, or pollen. the airways narrow and produce excess mucus, making it difficult to breathe. Chronic lower airway inflammation is known to be more common in individuals that also have inflammatory disorders of the upper airway. the scientific understanding of asthma continues to improve and it is important for providers who treat upper or lower airway inflammation to be familiar with asthma's definition and pathophysiology.

Pathophysiology Asthma Airway

Comments are closed.